What is Inflammatory Bowel Disease? Causes, Symptoms and Treament!
Managing Inflammatory Bowel Disease IBD:
1. What Is IBD?
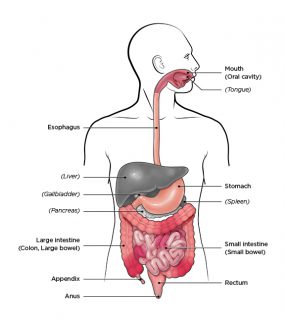
Inflammatory bowel diseases”IBD” are a group of inflammatory conditions in which the body’s own immune system attacks parts of the digestive system. The two most common inflammatory bowel diseases are Crohn’s disease (CD) and ulcerative colitis (UC). IBD affects as many as 1.4 million Americans, most of whom are diagnosed before age 35. There is no cure for IBD but there are treatments to reduce and control the symptoms of the disease. IBD
CD And UC,
cause chronic inflammation of the GI tract. CD can affect any part of the GI tract, but frequently affects the end of the small intestine and the beginning of the large intestine. The inflammation in CD can affect all layers of the intestinal lining.
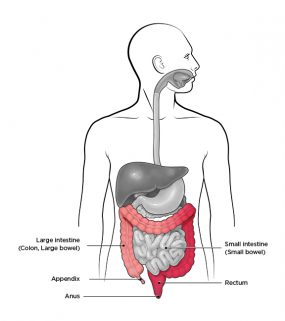
Ulcerative colitis (UC) is characterized by inflammation in the large intestine (colon) and the rectum. The inflammation in UC occurs only in the innermost layer of the intestinal lining.
2. Symptoms of IBD:
The symptoms of IBD vary from person to person and may change over time. The most common symptoms for CD and UC are frequent and/or urgent bowel movements, diarrhea, bloody stool, abdominal pain, and cramping.
People with IBD may also report symptoms such as fatigue, lack of appetite, and weight loss. IBD is characterized by times of active disease (flares) when symptoms are present, and times of remission when little or no symptoms are present.
- Diarrhea.
- Fever and fatigue.
- Abdominal pain and cramping.
- Blood in your stool.
- Reduced appetite.
- Unintended weight loss.
3. Causes Of IBD:
The exact cause of IBD remains unknown. Researchers believe that a combination of four factors leads to IBD:
- A genetic component.
- An environmental trigger.
- The imbalance of intestinal bacteria.
- And an inappropriate reaction from the immune system.
Immune cells normally protect the body from infection, but in people with IBD, the immune system mistakes harmless substances in the intestine for foreign substances and launches an attack, resulting in inflammation.
4. Risk Factors of IBD:
As many as 60,000 new cases of IBD are diagnosed in the United States each year.
- Age: IBD can occur at any age, but often people are diagnosed between the ages of 15 and 35.
- Gender: In general, IBD affects men and women equally.
- Ethnicity: IBD is more common among Caucasians, but it can affect people of any racial or ethnic group.
- Family history: As many as one in five people with IBD have a first-degree relative (parent, child, or sibling) with the disease.
- Cigarette smoking: Smokers are more likely to develop CD.
- Where you live. If you live in an industrialized country, you’re more likely to develop IBD.
5. Types of IBD include:
-
A. Ulcerative Colitis:
- This condition causes long-lasting inflammation and sores (ulcers) in the innermost lining of your large intestine (colon) and rectum.
-
B. Crohn’s Disease:
- This type of IBD is characterized by inflammation of the lining of your digestive tract, which often spreads deep into affected tissues.
6. Diagnosis Of IBD:
To help confirm a diagnosis of CD or UC, one or more of the following tests and diagnostic procedures may be performed.
A. Blood Tests:
The presence of inflammation in the body can be identified by examining the levels of several factors in the blood, including red and white blood cells, platelets, and C-reactive protein (CRP).
Tests may be performed to help healthcare providers differentiate IBD from non-IBD and CD from UC (ex., IBD Diagnostic). In certain situations, blood tests may also be used to evaluate a patient’s risk of developing disease complications, as well as to optimize treatment strategies (ex., Crohn’s Prognostic test).
B. Stool Tests:
Stool tests look for signs of inflammation in the GI tract as well as infections.
C. Endoscopic:
This procedure utilizes a flexible tubular camera to look inside of the digestive tract by entering through the mouth or anus. The scope has other tools that may be used for additional purposes, including the collection of tissue samples or biopsies.
- Capsule endoscopy may also be performed.
- This involves swallowing a capsule equipped with a camera (PillCam, Endo Capsule) that takes pictures as it travels through the intestine.
- The images are wirelessly sent to a receiver worn by the patient.
- The capsule is expelled during a bowel movement, usually within a day.
D. External Imaging:
These procedures utilize different technologies to generate images of the digestive organs and other soft tissue from outside the body, including computerized tomography (CT) scans and magnetic resonance imaging (MRI).
| Crohn’s Disease | Ulcerative Colitis |
|---|---|
| Can affect any part of the GI tract (from the mouth to the anus)—Most often it affects the portion of the small intestine before the large intestine/colon. | Occurs in the large intestine (colon) and the rectum. |
| Damaged areas appear in patches that are next to areas of healthy tissue. | Damaged areas are continuous (not patchy) – usually starting at the rectum and spreading further into the colon. |
| Inflammation may reach through the multiple layers of the walls of the GI tract.
Sources: https://www.cdc.gov |
Inflammation is present only in the innermost layer of the lining of the colon. |
7. Complications:
Complications from IBD can include:
- Anemia.
- Arthritis.
- Weak bones.
- Eye problems.
- Inflammation of the liver.
- Skin ulcers.
- Kidney stones.
- And among children, stunted growth and delayed puberty.
These are largely due to the impaired functioning of the intestines in absorbing nutrients from ingested food. Arthritic pain is related to inflammation outside of the digestive tract. Patients with IBD are also at an increased risk of colon cancer. However, many people with IBD and that with proper treatment and lifestyle changes can live normal, fulfilling lives.
8. Treatment Of IBD:
- Treatment of IBD usually focuses on the management of its symptoms through medications.
- The drugs used for controlling inflammation include aminosalicylates, corticosteroids, and immunomodulators.
- Antibiotics are usually prescribed to patients with Crohn’s disease, but not to those with ulcerative colitis.
- If the symptoms do not respond to medications, then surgery may be performed to mend or remove damaged portions of the intestine.
Fortunately,
There are many different treatments available to people living with inflammatory disease, and if you are hoping for natural herbal remedies, you will be happy to hear that some of the most effective treatments for IBD are, in fact, herbal in nature.
Your primary physician or specialist can prescribe medications to you that will definitely help with your symptoms, but many IBD sufferers find that the associated side effects with these medications are not worth the relief they get and instead turn to more effective natural remedies that aren’t saddled with those same issues.
The Most Effective,
Natural treatments for inflammatory bowel disease will include diet changes and supplements designed to rebuild and repair damaged intestinal tissues. When combined correctly, diet changes and these supplements can not only bring you relief from your pain and other symptoms.
But reverse any physical damage that the disease has inflicted in your body by replacing damaged tissues with new, healthy mucosal linings. An experienced naturopath will be able to consult with you to build a great treatment plan designed specifically for you and get you on the road to recovery in no time.
In Crohn’s Disease,
When surgery is performed, a conservative approach is generally adopted, to keep as much of the gut intact as possible. After an operation, your doctor may recommend that you take maintenance therapy, as this is shown to reduce the chance of the disease returning in the future.
You should discuss this with your gastroenterologist. It is not recommended to stay off therapy after an operation for Crohn’s disease unless you are having regular reviews to ensure any recurrent disease is promptly attended to.
I. Diet and Nutrition:
IBD and IBS are not caused by diet. However, diet can affect symptoms. Once IBD and IBS have developed, paying special attention to what is eaten may go a long way toward reducing symptoms and promoting adequate nutrition.
There is no diet or eating plan that will result in improvement for everyone with IBD or IBS. Dietary recommendations must be individualized, depending on the disease and the part of the intestine that is affected. Furthermore, these diseases change over time, and eating patterns should change accordingly.
The key is to strive for a well-balanced, healthy diet,
- It is important to remember that it is not just the amount of food eaten that guarantees a healthy diet, but daily intake needs to include an adequate amount of calories and nutrients.
- A balanced diet should contain a variety of foods from all food groups.
- For a listing of sample foods and beverages to potentially try and avoid.
- It is also important for people with IBD or IBS to pay attention to fluid intake.
- When chronic diarrhea is present, it can lead to dehydration.
- Stay well hydrated to avoid complications.
During periods of disease are-ups, eating may cause abdominal discomfort and cramping.
Here’re Some Ways to Reduce These Symptoms:
- Eat smaller meals at more frequent intervals: Eat ve small meals a day, every three or four hours, rather than the traditional three large meals a day.
- Reduce the amount of greasy or fried foods. High-fat foods may cause diarrhea and gas if fat absorption is incomplete.
- Watch dairy intake: Persons who are lactose intolerant or who are experiencing IBD or IBS may need to limit the amount of milk or milk products they consume.
- Restrict the intake of certain high-fiber foods: If there is a narrowing of the bowel, these foods may cause cramping. High-fiber foods also cause contractions once they enter the large intestine. Because they are not completely digested by the small intestine, these foods may also cause diarrhea.
Avoid,
- Problem (trigger) foods: Eliminate any foods that make symptoms worse. These may include “gassy” food (such as beans, cabbage, and broccoli), spicy food, popcorn, and alcohol, as well as foods and drinks that contain caffeine, such as chocolate and soda.
II. During IBD Symptoms:
A. Foods Beverages to Try:
- Bananas, applesauce, canned varieties of fruit.
- White bread, crackers made with white flour, plain cereals.
- White rice, re ned pasta.
- Potatoes without the skin.
- Cheese (if you’re not lactose intolerant).
- Smooth peanut butter.
- Bland soft foods.
- Cooked vegetables.
- Broth.
- Broiled or steamed sh (e.g., herring, salmon, halibut, flounder, sword sh, or pollack).
- Canola and olive oils.
- Low-sugar sports drinks and Crystal Light diluted with water.
B. Food Beverages to Avoid:
- Fresh fruit (unless blended or juiced).
- Prunes, raisins, or dried fruit.
- Uncooked vegetables and raw foods.
- High- ber foods (such as ber-rich bread, cereals, nuts, and leafy greens).
- High-sugar foods.
- Skins, seeds, popcorn.
- High-fat foods.
- Spicy foods.
- Beans.
- Some dairy products.
- Large food portions.
- Caffeine in coffee, tea, and other beverages.
- Ice-cold liquids (even water).
It is always important to keep a food journal to help understand which foods can be tolerated and not tolerated during the time of a are.
9. Medications:
There are five main categories of medications used to manage the disease and its symptoms:
I. Aminosalicylates:
- Such as sulfasalazine, mesalamine, olsalazine, and balsalazide, are medicines containing 5-aminosalicylic acid, an aspirin-like compound.
- They reduce inflammation in the lining of the intestine and are used in mild to moderate cases.
II. Corticosteroids:
- Including budesonide, prednisone, and prednisolone are steroids that are used as a short-term treatment during flares.
- They act on the immune system and suppress its ability to begin and maintain inflammation.
III. Immunomodulators:
- Such as azathioprine, 6-MP, cyclosporine, and methotrexate, affect the body’s immune system so that it is unable to maintain an inflammatory response.
- Unlike steroids, however, they are a long-term treatment.
IV. Biologic Therapies:
including infliximab, adalimumab, certolizumab pegol, golimumab, vedolizumab, and natalizumab, are antibodies grown in the laboratory that stop certain proteins in the body from causing inflammation.
V. Antibiotics:
Such as metronidazole and ciprofloxacin, are used when infection occurs, either from the disease itself or from post-surgical procedures.
10. Probiotics:
Probiotics are live bacteria that are similar to beneficial (often called “good” or “friendly”) bacteria that normally reside in the intestines. Under normal circumstances, beneficial bacteria keep the growth of harmful bacteria in check.
If the balance between good and bad bacteria is thrown off, causing harmful bacteria to overgrow, diarrhea and other digestive problems can occur. Probiotics can be used to restore the balance of these “good” bacteria in the body.
They Are,
available in the form of dietary supplements (capsules, tablets, and powders) or foods (yogurt, fermented and unfermented milk, miso, tempeh, and some juices and soy beverages). There is no strong evidence to suggest that the use of probiotics may help people with IBD or IBS, but some people think it helps. More research is needed. Those interested in using probiotics should discuss this with their health care provider.
11. Pain Management:
Pain can be a serious issue for patients. Two forms of psychotherapy -cognitive-behavioral therapy (CBT) and hypnotherapy- have the most support in being clinically effective in reducing pain as well as the frequency, intensity, and duration of IBD and IBS symptoms.
A. CBT:
has shown promise for patients with moderate to severe IBD and for those with IBS who also suffer from anxiety or mood disorders. CBT can help patients learn coping strategies to control the symptoms brought on by anxiety.
B. Hypnotherapy:
Hypnotherapy is one of the most successful treatment approaches for chronic IBS, both in the short term and the long term. Studies suggest that in addition to decreasing pain perception at the level of the brain, hypnosis may improve immune function in IBD and IBS, increase relaxation, reduce stress, and ease feelings of anxiety.
C. Non-Steroidal Anti-Inflammatory Drugs:
(NSAIDs) are commonly used to treat abdominal pain and musculoskeletal symptoms associated with IBD. However, multiple studies have demonstrated that NSAIDs may increase the risk for IBD relapse, flares, and an overall increase in disease activity.
12. Inflammatory Bowel Disease in Children:
- IBD is uncommon in children but does occur. Children with IBD develop the same symptoms as adults.
- However, untreated IBD can lead to delayed or impaired growth and it is important to keep inflammation under control to prevent this.
- The treatment of children with ulcerative colitis or Crohn’s disease is very similar to that of adults with IBD.
Can People With IBD Lead a Normal Life?
The vast majority of people with IBD lead useful and productive lives, even though they need to take medications. When their disease is in remission, they feel well and are usually free of symptoms. People with IBD marry, engage in sexual activity and have children. They hold down jobs, care for families, and enjoy sport and recreational activities.
Even though there is no cure for IBD, current medical therapy has improved the health and quality of life of most people with ulcerative colitis and Crohn’s disease. There is a good reason to believe that research underway today will lead to further improvements in the medical and surgical treatment of inflammatory bowel disease.
If you find this article useful, don’t forget to share it with your friends and family, as you might help someone in need. Thanks.
Disclaimer: “Nothing in this article makes any claim to offer cures or treatment of any disease or illness. If you are sick please consult with your doctor.”
References